Pelvic Organ Prolapse and How Pelvic Floor Therapy Can Help
The diagnosis of pelvic organ prolapse may initially seem scary. It can be easy to go down the google rabbit hole and find the worst possible outcomes on the internet. However, we want you to know that the diagnosis of pelvic organ prolapse doesn’t automatically mean your doom. There ARE strategies to help address the symptoms of pelvic heaviness and to potentially reduce the need for surgery in the future.
First of all, what is Pelvic Organ Prolapse?
The pelvic floor is made up of layers of muscle and connective tissue that come together to create a cradle of support for the pelvic organs including the bowel, bladder, uterus, cervix, vagina, urethra, and rectum. Pelvic organ prolapse, also known as POP, occurs when the pelvic floor muscles or pelvic ligaments weaken, allowing one or more of the pelvic organs to slip from their original position in the body down into or out of the vagina.
The type of pelvic organ prolapse occurring depends on which pelvic organ is affected. The most common types of pelvic organ prolapse include:
Cystocele – when the bladder drops into or out of the vagina (also called “dropped bladder”)
Rectocele – when the rectum bulges into or out of the vagina
Uterine Prolapse – when the uterus bulges into or out of the vagina (also called “dropped uterus”)
Pelvic organ prolapse (POP) when defined by symptoms, has a prevalence of 3-6% and up to 50% when based upon vaginal examination in women in the United States. (1) It may or may not be accompanied by another pelvic floor disorder such as urinary or fecal incontinence. POP remains one of the most common pelvic floor disorders treated by pelvic floor physical therapists.
Symptoms of Pelvic Organ Prolapse
Some common symptoms of pelvic organ prolapse include:
A bulge or “something coming out” of the vagina that can be seen or felt
Pelvic discomfort during exercise or sex
A feeling of pressure or fullness in the pelvis
Urinary incontinence
Difficulty passing stool
Difficulty inserting tampons
Common Causes of Pelvic Organ Prolapse
As mentioned previously, POP is usually the result of weakened or damaged pelvic floor muscles and/or pelvic ligaments. Some of the most common causes of this are:
Vaginal childbirth(s)
Chronic intra-abdominal pressure (including from obesity, frequent straining during bowel movements, and chronic cough especially due to ongoing health conditions such as COPD)
Giving birth to a baby weighing 8.5 lbs or more
History of abdominal surgery
Aging (most women experiencing pelvic organ prolapse are aged 60 and older)
Menopause-induced hormonal changes, particularly estrogen loss
Family history of pelvic organ prolapse or connective tissue disorders
Diagnosis and Treatment of Pelvic Organ Prolapse
Pelvic organ prolapse can be diagnosed via a physical exam in which your provider may look and feel for a bulge in the vaginal canal. They may get a more accurate diagnosis by having you stand up during the assessment, in order to see what it looks like against gravity. Your provider may also assess any accompanying symptoms you may be having such as urinary incontinence or inability to fully empty your bladder.
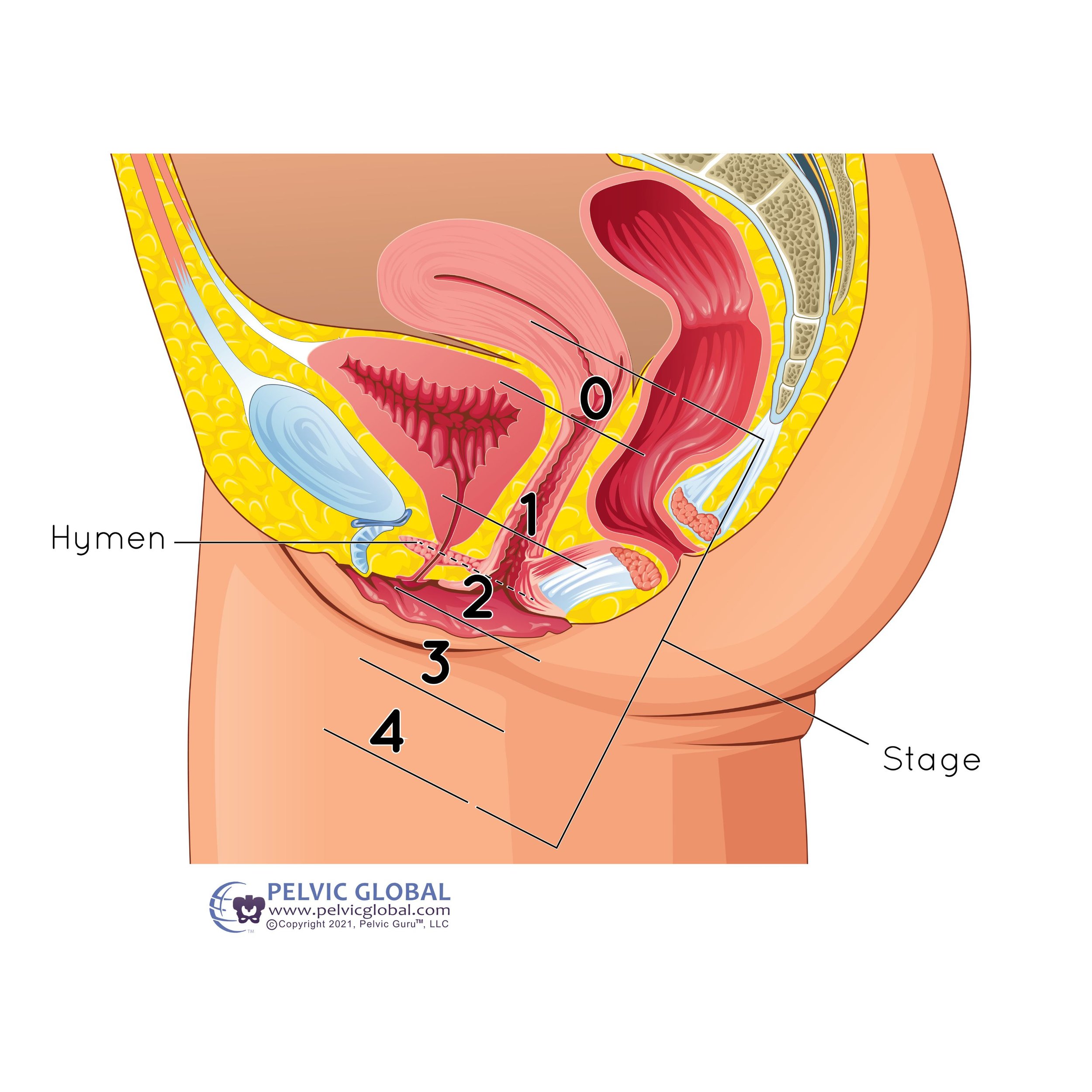
Pelvic organ prolapse is assessed from stage 0 to stage 4 depending on how far the pelvic organ has descended into the vagina.
Stage 0 – no descent
Stage I – the pelvic organs have dropped into the upper part of the vagina but are still somewhat supported by the pelvic floor
Stage II – the pelvic organs have dropped into the lower part of the vagina but have not descended outside the vagina
Stage III – the pelvic organs have dropped past the vaginal opening and are protruding
Stage IV – the pelvic organs have descended completely through the vaginal opening
The extent of treatment for your pelvic organ prolapse is dependent on the type of prolapse and extent of symptoms as well as other factors such as the ones listed above.
Treatment of prolapse may include one or more of the following:
Pelvic floor therapy to strengthen and coordinate the pelvic floor muscles, manage intra-abdominal pressure and address accompanying symptoms of pelvic organ prolapse
Pessary, a removal device that is inserted into the vagina to help provide support to the pelvic organs. This can be a great adjunct to pelvic floor therapy!
Diet modification including increasing fiber intake to prevent constipation and reduce straining during bowel movements
Surgery to create more support for the pelvic floor using an individual’s own tissue or synthetic tissue; this is often a solution used for women who have more severe prolapse and who are still sexually active
Pelvic Floor Therapy for Pelvic Organ Prolapse
The first-line treatment for lower grade pelvic organ prolapse is pelvic floor physical therapy. (2) There is level 1, grade A evidence to recommend pelvic floor therapy and studies show that women who perform pelvic floor muscle therapy for the treatment of POP have a significant reduction in symptoms!
Because a common cause of prolapse is intra-abdominal pressure which can result from poor coordination of the pelvic floor, diaphragm and core, pelvic floor therapy is an effective and noninvasive approach to treating pelvic organ prolapse. Pelvic floor therapy can also address many of the uncomfortable symptoms accompanying pelvic organ prolapse such as urinary incontinence, constipation, abdominal pressure, lower back pain, and pelvic fullness or heaviness.
Some interventions your pelvic floor physical therapist may use in treating POP include:
Manual Therapy, which is the utilization of soft tissue mobilization and manipulation to help the pelvic floor maintain appropriate tension/relaxation
Introducing good bladder and bowel habits – to improve function of the pelvic floor and bladder and help decrease pressure on the pelvic floor by improving bowel emptying
Intra-Abdominal Management Training – to help manage the pressure throughout the day during daily activities and exercise to prevent placing excessive stress on the pelvic floor
Strengthening Exercises – for the pelvic floor muscles and for the whole body in order to allow for even weight and load distribution when moving and lifting throughout day to day activities.
Conclusion
The big question we often get is: Is pelvic organ prolapse reversible? Because reversible means, “back to the state it once was”, the short answer is no. But can it get better? YES. Pelvic floor therapy is shown to help reduce the symptoms of heaviness and bulging, help improve an individual’s function and performance of every day activities and exercise, and improve symptoms of urinary or fecal leakage.
While it is impossible to reverse what has already been done (i.e. factors that influence pelvic organ prolapse such as pregnancies, genetics, bowel and bladder behaviors, hormonal changes, heavy lifting activities etc.), we can focus on what we CAN control, which is getting stronger, working towards becoming more active and finding acceptance and moving forward with support.
We are here to help you. If you are finding you are experiencing symptoms of pelvic organ prolapse and would like some direction and support, feel free to send us a message or schedule an evaluation!